Deployment
Following the terrorist attacks in the USA on 11 September 2001 (now commonly referred to as '9/11'), Britain deployed its armed forces to Afghanistan alongside the US and other allies. Their mission was to destroy al-Qaeda - the group behind the attacks - and the Taleban regime which supported them.
The Taleban was quickly overthrown and soldiers turned their attention to peacekeeping and reconstruction projects. By 2004, however, a re-organised Taleban had stepped up their attacks on the new Afghan government's security forces and on the international coalition's troops.
In April 2006, the British Army redeployed in strength, focusing on the southern province of Helmand. Over 3,000 troops were sent to help with reconstruction and security efforts. They operated out of Camp Bastion, a purpose-built base in the desert near the provincial capital, Lashkar Gah.
Camp Bastion Hospital
In April 2006, Hospital Squadron of 22 Field Hospital arrived at Bastion and set up a 25-bed tented structure. This could expand to 86 beds, if needed. Separate tents, with inter-connecting corridors, were erected for operating theatres, wards, an X-ray department and an emergency department. These were the humble beginnings of Camp Bastion Hospital.
In February 2008, ten months later than planned, work was completed on upgrading the hospital from a Tier 1 temporary tented facility to a Tier 2 semi-permanent purpose-built structure. This enabled logistical adjustments that turned out to be lifesaving.
The ‘Right Turn Resuscitation’ process was introduced, meaning critically injured patients were taken straight into the operating theatre to the right when they entered the hospital, rather than waiting for assessment in the emergency department.
‘It’s like a ballet’
Interviewed in 2013, Major Patsy Beesley, Queen Alexandra's Royal Army Nursing Corps, describes the co-ordinated teamwork of the Camp Bastion Hospital staff.

Nurses at Camp Bastion hospital, 2007
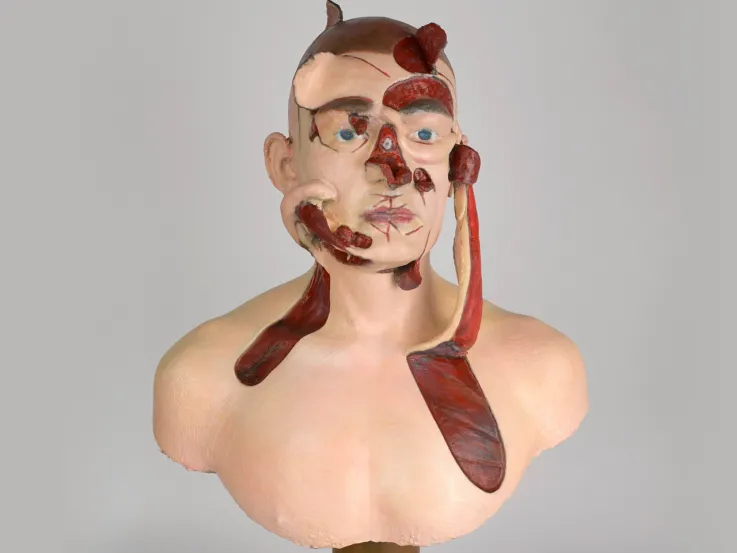
Injuries
One of the main threats to soldiers and civilians in Afghanistan came from IEDs. These killed 224 British soldiers and seriously wounded many more.
For medical staff on their first deployment, the severity of the IED-related injuries seen at Camp Bastion Hospital was something they were unlikely to have experienced at their NHS practices. Missing limbs, significant and visible tissue loss, as well as substantial internal blast injuries were common and meant major trauma patients were routine.
‘Where do you start?’
Interviewed in 2013, Major Thomas Konig, Royal Army Medical Corps, discusses the injuries caused by IEDs.
Unsurprisingly, witnessing such injuries and dealing with the death of soldiers and civilians had an effect on the hospital staff. Interviewed in 2016, Sergeant Chantelle Taylor, Royal Army Medical Corps, explains.
Intense work
Camp Bastion Hospital was the busiest hospital in Afghanistan. Between April and October 2008, it admitted 1,049 patients. Interviewed in 2013, Major Chantel Whelan, Queen Alexandra's Royal Army Nursing Corps, outlines the commitment and hard work required.
Attacks
Camp Bastion was attacked several times. One of the worst incidents was the Taleban raid on 14 September 2012, which killed two US Marines and destroyed or damaged several aircraft before the raiders were killed or captured.
This threat meant that all personnel, including medical staff, had to wear body armour during alarms and to take part in regular training drills.
Body armour
Interviewed in 2013, Major Patsy Beesley describes wearing protective clothing while serving at Camp Bastion.
FOBs
Outside of Camp Bastion, individual medics were regularly deployed with British Army units. By 2007, the guerrilla nature of encounters with the Taleban meant that Forward Operating Bases (FOBs) needed to be established in hostile zones.
Medical troops worked at these bases and also accompanied British soldiers when they were drawn into heavy firefights in towns like Musa Qala and Sangin. Other medics worked at regional medical centres such as the one at Lashkar Gah, treating both soldiers and Afghan civilians.
Training
Formations such as 16 Air Assault Brigade also built medical training into their pre-deployment preparation. The aim was to train every fourth soldier in front-line infantry units to the level of team medic.
This meant they would be able to provide vital medical care for the first 15 minutes after injury, giving combat medical technicians from Close Support Medical Regiment time to reach them from Camp Bastion or a FOB.
Combat medics
Team medics proved generally effective. However, it would often take longer than 15 minutes to get a helicopter out to the troops on the ground.
This later led to combat medical technicians always being attached to foot patrols and road convoys.
Patrolling
Interviewed in 2013, Corporal Graeme Harding, 16 Close Support Medical Regiment, Royal Army Medical Corps, describes the qualities needed by medics when on patrol in Helmand.
IED
Interviewed in 2012, Lance Corporal Chris Schivas, 16 Close Support Medical Regiment, Royal Army Medical Corps, describes a narrow escape during a vehicle patrol in Kajaki, Helmand.
Evacuation
Evacuating casualties by road was dangerous and almost impossible due to the high number of IEDs planted by the Taleban. The safest way to get casualties from the field to Camp Bastion Hospital was to have them flown out by the medical emergency response team (MERT), usually by Royal Air Force CH-47 Chinooks.
This method was introduced soon after the deployment to Helmand. By 2007, in-flight blood transfusions could be carried out. From 2008, anaesthetists and emergency physicians accompanied most teams.
MERT
Interviewed in 2013, Colonel Peter Mahoney, Royal Army Medical Corps, describes working as a consultant on Medical Emergency Response Team flights to Camp Bastion Hospital.
Emergency care
While patrols waited for helicopters to arrive to evacuate the wounded, the attached Royal Army Medical Corps combat medics or the infantry team medics did their best to care for them.
This often involved stabilising casualties by applying tourniquets and field dressings to reduce blood loss and applying pain relief.
Multiple casualties
Interviewed in 2007, Corporal Paul Hartley, 16 Close Support Medical Regiment, Royal Army Medical Corps, describes dealing with multiple injuries in Kajaki, Helmand.
TMC
In 2011, the British signalled their intention to end all combat missions in Afghanistan by December 2014. As part of this gradual withdrawal, a new troop medical centre (TMC) was established at Camp Shorabak, adjacent to Camp Bastion. It had a ward accommodating 20 beds, a primary healthcare facility and two resuscitation bays.
US and Danish mentors were based there and the deployed medical director from Camp Bastion Hospital attended ward rounds every other week with Afghan National Army surgeons. Regular ‘train the trainer’ sessions were held there and at Bastion.
Legacy
This training policy established Bastion’s legacy, enhancing the skills of those locals working at the TMC to treat casualties, and enabling the gradual transfer of Afghan National Security Forces personnel and Afghan civilians to the facility.
In 2014, all bases were gradually closed and medical support outside Bastion ended. The British hospital at Bastion was closed on 22 September, and the British combat mission in Afghanistan finally ended on 26 October 2014 with the handover of Camp Bastion to Afghan forces.